East Melbourne VIC 3002
Types of Contraception: Know Your Options

When we talk about contraception, we are discussing methods and techniques to prevent a pregnancy. In the past, this was commonly called family planning. We now realise that sexually active women who wish to avoid an unwanted pregnancy require counselling concerning the value and options available with respect to contraception. This counselling primarily takes into account the wishes and needs of the woman and may or may not involve a partner.
What Is the Best Contraception?
There are numerous options when it comes to contraception. The choice of a particular contraceptive method requires careful consideration and counselling. Information concerning each contraceptive method needs to be presented and the pros and cons discussed.
Each patient needs to be treated as an individual with their own wishes and needs when it comes to contraception and reproduction.
Types of Contraception: Know Your Options
It’s important to be aware of the types of contraception available to you.
There are around 12 methods of contraception available catering to different bodies and lifestyles. Contraceptive methods readily available range from hormonal solutions, non-hormonal, emergency contraceptive options to permanent contraception solutions.
So, what types of contraception are there?

Condoms
A condom is usually made of latex or a similar plastic material. It is made to cover the penis during intercourse and therefore prevents the flow of sperm into the canal of the cervix or neck of the womb and prevents pregnancy. It is also shown to reduce but not totally negate the chance of acquiring a sexually transmitted disease.

Female Condoms
A much less common device is a female condom which is a plastic or latex device fitted into the upper vagina to also act as a barrier. A female condom is more commonly associated with spillage of sperm and as such, may be more awkward to use and acts less as a barrier. Except for the possibility of being allergic to latex, there are no side effects associated with these devices.
Barrier forms of contraception as mentioned, also suggests that you are practicing safe sex. Perhaps the best way to reduce the risk of sexually transmitted diseases is to use condoms to prevent the spread of infection.

Combined Oral Contraceptive Pills or Hormonal Vaginal Rings
Contraceptive pills and vaginal rings contain the two female hormones, oestrogen and progesterone which act by a feedback mechanism to prevent ovulation by turning off the brain-controlled system that stimulates the hormone changes leading to ovulation. The pill can be taken orally or the hormones can also be absorbed through the vagina using a vaginal ring (NuvaRing).
In the past, contraceptive pills contained synthetic oestrogen and synthetic progesterone. More recently, pills have been designed that contain both a purely natural oestrogen and a low risk from side effects type of progesterone.
By placing 24 active pills in the packet along with 4 sugar pills (in the past it was 21 and 7) this reduces the length of the withdrawal bleed that simulates a period. It is possible to skip periods altogether by not taking any sugar tablets. This means that you only take the active hormone tablets. This has no effect on your general wellbeing and has no effects on your fertility. In fact, if you have significant period problems such as heavy periods, painful periods or an exaggerated form of premenstrual syndrome called premenstrual dysphoria disorder, skipping periods may be a useful form of treatment.

Contraceptive Pill
There are absolute and relative contraindications to the pill and possible side effects of the pill. Absolute contraindications to the pill which means you should not use combined oral contraceptives at all, include hormone dependent cancers, previous blood clotting disorders and previous significant side effects such as migraine.
Possible side effects of the pill vary enormously between women. These include:
- Breast soreness
- Bloating
- Mood changes
- Headaches or migraine
- Nausea
- Anxiety
- Insomnia
- Fluid retention
- Diarrhoea or constipation
- The development of blood clots
- Hypertension (high blood pressure)
The effectiveness of the pill is thought to be 99.6%. Failures with respect to contraception can occur if the pill is not absorbed such as when you have gastroenteritis or you take another pharmaceutical which interferes with the absorption of the pill such as antibiotics. Obviously forgetting to take the pill also can lead to failure. When side effects do occur with respect to the pill it is possible to negate these side effects by changing to another hormone combination; that is changing the brand of pill that you are using.
More recently progesterone only pills that also inhibit ovulation have come on to the market. As a number of the side effects of the pill are due to the oestrogen hormone, therefore the use of progesterone only pills may be particularly beneficial to some women.

Contraceptive injections
Depo-Provera has been available for some time. This also inhibits ovulation and is an injectable progesterone hormone that lasts for 3 months. This form of contraception was found to be particularly useful where women would forget to take the pill.
Side effects of contraceptive injections include irregular bleeding and mood changes were found to be common and the problem then arose that these side effects would last for the full 3 months and were difficult or impossible to reverse.
With the advent of better oral contraceptives and other contraceptive techniques Depo-Provera has become less popular.

Contraceptive Implants
Contraceptive implants In Australia is a small plastic rod placed under the skin on the inside of your arm between your biceps and triceps muscles. This has shown to be an effective form of contraception.
Contraceptive implants release a progesterone hormone which again, inhibits ovulation much as the combined oral contraceptive pill does. The rods last for 3 years and have no long-term effect on your fertility. It may lead to irregular bleeding or you may notice that your period disappears altogether as again, it suppresses the release of the hormones produced by your brain that control your menstrual cycle.
If you develop any of the complications associated with the use of this device it is simple to remove it in a doctor’s office.
Common side effects include:
- Mood changes
- Bloating
- Breast soreness
- Fluid retention
All progesterone forms of contraception are safe to use while you are breastfeeding as it is only the oestrogen hormone that interferes with lactation.

Low Dose Progesterone Only Pills (The Minipill or Breastfeeding Pill)
A low dose or mini-dose progesterone pill is often used by breastfeeding women to provide contraception as it does not interfere with lactation. It is not as reliable in preventing pregnancy as the combined pill when it is used in non-lactating women.
If you are using progesterone only contraception because you have side effects when you take oestrogen, it is better to use the new high dose progesterone alternatives.
Because of the low dose of these contraceptive pills, it is important that they are taken at the same time every day and it is also important that you do not miss taking a pill as then pregnancy is more likely.
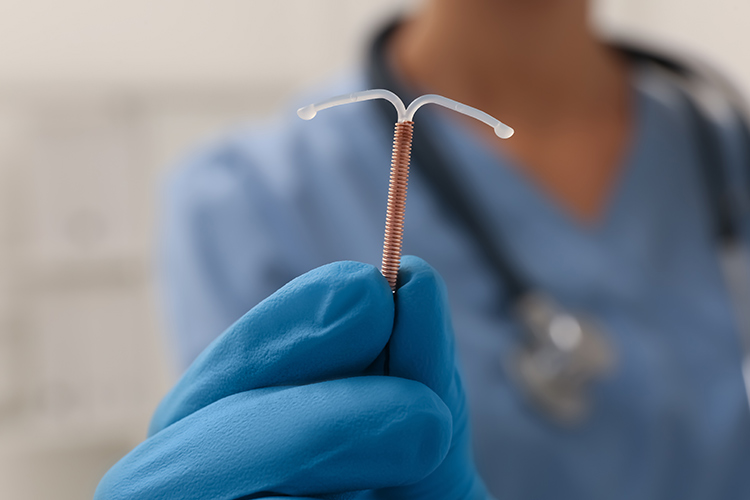
Intrauterine Devices (IUDs)
Intrauterine devices have been a contraceptive for over 50 years. Intrauterine devices involve placing a small device within the uterine cavity to prevent implantation of a fertilised egg.
The most popular forms of IUDs contain and secrete a steady dose of progesterone hormone. There are two types of progesterone IUDs currently available. One is a Mirena IUD which secretes a larger dose of progesterone and the second is a smaller device called a Kyleena. A Kyleena secretes a lower dose of progesterone hormone and is easier to insert because of its smaller size. Especially in women who have not had a child but are less satisfactory in controlling heavy and painful periods because of the lower dose of hormone.
These devices reduce the pregnancy rate as the progesterone released into the uterus results in a uterine lining which is even less conducive to implantation of a fertilised egg. The lining of the uterus is thinned out by the progesterone hormone and in at least 50% of women periods disappear altogether because of the thin lining which provokes no bleeding at all when a period is due.
Side Effects of IUDs
Side effects of progesterone hormone released into the uterus result from the small amount that is absorbed into your bloodstream.
These side effects may and are often temporary such as:
- Breast soreness
- Bloating
- Mood changes
- Hair loss – This is a particularly uncommon side effect of hair loss but this side effect often persists and may be an indication to remove the IUD.
Non-hormone releasing IUDs are small and often easier to introduce into the uterus. However, Mirena IUDs especially can be used to treat painful, heavy periods; non-hormone releasing IUDs often have the reverse effect and may make your periods heavier and more painful. Because of this non-hormone releasing IUDs have become relatively unpopular.
All IUDs can be associated with irregular bleeding or spotting. It is not uncommon to spot for some weeks after the insertion of a progesterone releasing IUD but the spotting almost always ceases or can be treated. Both progesterone releasing and non-hormonal IUDs have an average lifespan of 5 years.
To find out more about IUDs, read our article about the Pros and Cons of IUDs

Permanent Forms of Contraception
All the above forms of contraception are reversible. That means if you cease using that particular method of contraception your fertility will return to its pre-existing state unless age is a factor.
Permanent forms of contraception should only be used if you are 100% certain that you do not want to conceive again. There are broadly two forms of permanent contraception.
Vasectomy
The vas is a tube that carries sperm that is released when a male ejaculates. If the vas is cut or divided then sperm will not be released during intercourse. The cutting of the vas is a surgical procedure which can be performed under local or general anaesthetic. As sperm have already been produced and are viable last for up to 3 months, a vasectomy will not be effective until 3 months after the surgical procedure and alternative contraception will be required. It is important to have a sperm test at 3 months post-surgery to ensure that the sperm count is zero. Reversing a vasectomy is not guaranteed to work and as mentioned, certainty is important with respect to future pregnancy not being wanted.
Tubal Ligation
This procedure is performed in women under general anaesthetic. A small telescope is inserted through the navel and usually clips are applied to both fallopian tubes so that the egg which is fertilised at the end of the tube (called the ampulla) cannot travel down in to the uterus and implant. More recently complete removal of the fallopian tubes on both sides (a bilateral salpingectomy) has been performed as an alternative. This is because it is estimated that 50% of ovarian cancers arise in the fallopian tubes so removing your fallopian tubes halves your risk of ovarian malignancy. Many women find this a more satisfactory alternative.
Natural Methods of Contraception
Natural methods of contraception rely on women predicting when they are fertile or ovulating. This may be indicated by a slight rise in temperature, usually of 1° Celsius or less or changes in cervical mucus where the mucus becomes more profuse and has a stringy quality. More recently there are urine test kits which predict ovulation by detecting the surge of hormone (LH) which triggers the release of the egg from the ovary. There may be difficulties in accurately determining when you are ovulating, especially if your cycle is irregular and unpredictable. In general, this form of contraception has a higher failure rate because of the inherent difficulties in detecting ovulation.
This form of contraception should be especially avoided if:
- You have an irregular cycle
- You have a fever or feel unwell due to a coexistent medical condition
- You undertake frequent overseas travel where you are crossing time zones
- You suffer from stress frequently which affects your menstrual cycle
- If you find it difficult to detect mucus changes at the time of ovulation
- If you are on a medication (such as antidepressants) which are known to interfere with your menstrual cycle
- Withdrawal – a male withdrawing his penis just prior to ejaculation may be used by couples as contraception. Because ejaculation can start to occur prior to it being recognised during intercourse, there is a significant failure rate in using withdrawal as your method of contraception.
Emergency Contraception
This form of contraception is often called the “morning after pill”. It is used when a couple have had unprotected sex and is used to prevent implantation of a fertilised egg. The success rate is usually over 90% if the emergency contraception is used within 5 days of unprotected sex. The sooner it is used after the episode the more reliable it is. There are two hormones that are used for emergency contraception and both are available at pharmacies without a prescription.
These two hormones are:
- Ulipristal – This is the better alternative as shown in a number of studies and is effective for up to 5 days after unprotected intercourse.
- Levonorgestrel – This is effective for up to 4 days after unprotected intercourse.
Because emergency contraception is not always effective, it is preferable to have a reliable form of contraception rather than simply relying on emergency contraception as your method of preventing pregnancy.

Which Contraception Should I Use?
As we can see from our discussion so far, there are numerous forms of contraception and all of them have pros and cons. It is important that you are seen as an individual, and that all your preferences and concerns are answered in an appropriate counselling session. The side effects as mentioned above, may point you in a certain direction. It may be important for you to try a form of contraception to see if it is appropriate for you. For example, no one knows if they will have side effects or issues using a contraceptive pill until you actually try it. There is no predictive test.
In some cases, a form of contraception is absolutely contraindicated and then you should be pointed in another direction. It is always important that you are reviewed after you start a form of contraception so that any issues or concerns can be addressed even if this is via a Telehealth conference.
What Types of Contraception Are Non-Hormonal?
Most forms of contraception include a hormonal component. The only forms of contraception that are non-hormonal, that have no hormone component at all include:
- Barrier methods such as condoms
- Non-hormonal containing IUDs
- Sterilisation procedures such as tubal surgery
- Natural methods of contraception – predicting ovulation
- Male contraception
There are a number of studies involving the production of a male contraceptive pill. No male contraceptive pills are as yet available but this deficiency in the market will probably be addressed within the next 5 years. Male contraceptive pills lower testosterone or male hormone levels but not to a level that would result in side effects in the majority of men.

When To See My Gynaecologist
General practitioners are well versed and extremely competent when it comes to discussing means of contraception. Where you have complex medical or gynaecological issues or you need to discuss more complex forms of contraception such as permanent forms of contraception, then you will need to see a gynaecologist.
This is especially if you have ongoing and significant symptoms of:
- Pelvic pain
- Bleeding abnormalities
- An abnormal cervical screening test
- Require an invasive form of contraception such as an IUD which may need to be inserted under a general anaesthetic
- Require permanent contraception such as a sterilisation procedure
Dr Kliman will discuss the pros and cons of every contraceptive option available, including non hormonal contraceptive options, natural contraceptive options as well as permanent solutions during your consultation.








