East Melbourne VIC 3002
Ten Common Signs And Symptoms That Indicate You Need To See A Gynaecologist

A Gynaecologist is a specialist who has had six years extra training in both obstetrics and gynaecology. Obstetrics involves the management of pregnancy. Gynaecology involves the management of signs, symptoms, abnormalities and concerns regarding the female reproductive system. All Gynaecologists must be a member of the Royal Australian and New Zealand College of Obstetricians and Gynaecologists. All Gynaecologists need to meet the stringent college requirements to show that they are up-to-date and have attended the appropriate meetings, conferences and educational content.
Over the last decade in particular, certain gynaecological subspecialities involving extra training in a certain field have been developed. These subspecialities include:
1. Oncology – gynaecological cancers
2. Urogynaecology – management of urinary incontinence and prolapse
3. Advanced laparoscopic surgery – keyhole surgery techniques to manage particularly severe cases of pelvic pain and endometriosis
4. Infertility and IVF
Many of the common signs and symptoms listed below can be managed by your local general practitioner. This includes having a cervical screening test and management of simple gynaecological concerns. There will be times however, where your symptoms are more concerning, may indicate the possibility of a gynaecological cancer or your symptoms and signs are persisting despite treatment. In this case, your general practitioner may refer you on to a specialist gynaecologist.
Gynaecological Signs And Symptoms That Indicate You Need To See A Gynaecologist
Abnormal uterine bleeding
Vaginal bleeding that is not in keeping with your normal menstrual cycle include intermenstrual bleeding or bleeding towards the middle of your cycle and postcoital bleeding or bleeding after intercourse. These indicate abnormal uterine bleeding and need to be investigated. In general, the older you become the more significant the symptoms may be as they are more likely to indicate a precancerous or cancerous lesion. History, examination and further tests may be indicated.
Pelvic Pain
Secondary pain or pain that has not been present since your period commenced, is an indicator of the development of new pathology including conditions such as pelvic infection or endometriosis. Pain that occurs with your period or with intercourse are especially signs of a gynaecological cause of the pain and these need to be investigated further and symptoms need to be controlled.
Heavy Menstrual Bleeding – Menorrhagia
Heavy menstrual bleeding can be a cause of iron deficiency anaemia, fatigue and general ill health. There are a number of possible causes. The commonest cause is called dysfunctional uterine bleeding which suggests that there is an abnormality of the cycle due to hormonal causes and this diagnosis implies no structural abnormalities such as fibroids or a condition called adenomyosis which is also a common cause of heavy bleeding.
Irregular Or Absent Periods
Irregular periods may be a sign that you are not ovulating. This may end up not having a significant cause and only needs to be treated if you are trying to conceive as it is impossible to conceive if you are not producing an egg. Absent periods may be a sign of the menopause and a premature menopause indicates that you have become menopausal or your ovaries have slowed down in their function prior to the age of 40. There are a number of other possible causes including unknown, thyroid disease, pituitary disease etc. and a wide number of investigations including a structural ultrasound may be necessary.
Premenstrual Dysphoria Disorder
Premenstrual dysphoria disorder is an important condition as it interferes significantly with the patient’s quality of life. The exact cause of this condition which is a severe version of premenstrual syndrome is unknown. However, depression, suicidal thoughts, anxiety, brain fog and an inability to socialise are all important symptoms. There are a wide variety of treatments and this condition should never be ignored as it can continue for some years and have a significant impact on a woman’s wellbeing.
Abnormal Vaginal Discharge with Or Without Itch And Irritation
There are a number of vaginal and vulval diseases associated with an abnormal discharge. This includes both infective conditions and immune disorders. An exact diagnosis with the appropriate tests is very important as these conditions can be ongoing and be associated with a significant impact on a woman’s quality of life. Appropriate testing and sometimes a biopsy is required and it is ideal to see a specialist with an interest in vulval and vaginal disorders. Gynaecologists with an interest in this field are included in the information provided by the ANZVS (Australian and New Zealand Vulva and Vaginal Society). Abnormal vaginal discharge is usually yellow, grey, green or blood stained. It can be excessive in amount, have an unpleasant odour or as mentioned, be associated with symptoms such as itch, irritation or pain.
Vulval Skin Disorders Associated With Itch, Burning Or Pain
There are a number of dermatoses or vulval skin disorders that are associated with the mentioned symptoms. It is possible to have a condition called vulvodynia where the skin is normal but the nerves in the skin are ‘over firing’ resulting in significant symptoms. However, there are also a number of infective disorders such as recurrent fungal infections and immune disorders such as lichen sclerosus, lichen planus and chronic dermatitis which can cause significant symptoms and often a biopsy taken under local anaesthetic will differentiate the possible causes.
Prolapse Symptoms Including Urinary Incontinence
A uterovaginal prolapse involves descent of the uterus itself or the bladder and bowel pushing into the vagina due to a deficiency in the strength and elasticity of the supporting tissue of the pelvis. This may occur for no obvious reason but may be associated with aging, difficult childbirth or genetic factors. An initial assessment is often made by a Gynaecologist who often will refer you on to a Gynaecologist specialising in this area called a urogynaecologist.
Infertility
Infertility is defined as failure to conceive after 12 months of trying to do so. In couples who are older, it may be worthwhile to investigate sooner and basic investigations include tests on ovulation, tests to ensure that the fallopian tubes are not damaged and are patent and a sperm test on the male partner. Furthermore, elaborate investigations may be needed. The initial investigations can be performed by a Gynaecologist but if there are ongoing issues and if IVF needs to be considered, then you will be referred to an infertility specialist who is a Gynaecologist with an interest and special training in this area.
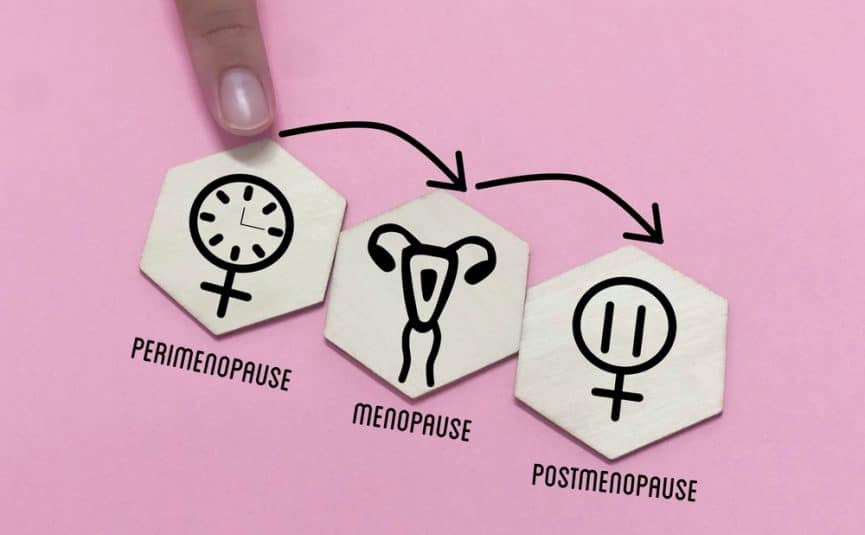
Menopausal Issues
As mentioned, the menopause is a slowing down of oestrogen production by your ovaries. This often occurs very gradually and the slow reduction is known as the perimenopause. Both in the perimenopause and the menopause itself, it is not uncommon to develop symptoms such as hot flushes, insomnia, brain fog, mood changes, vaginal dryness or loss of libido. Osteoporosis may start to develop due to oestrogen deficiency and it is important that you have basic health checks such as an appropriate mammogram and a bone density study. The pros and cons of menopausal hormone therapy will be discussed through your general practitioner or your Gynaecologist. It is important not to ignore any concerns as symptoms may last for some years. There is a significant amount of unscientific inappropriate information on the internet and this often makes management of the menopause more complex. It is especially important not to listen to anecdotal information or information provided well meaning relatives.
Associate Professor Len Kliman has been a specialist Gynaecologist for over 35 years and has managed all of the above symptoms or in the case of conditions such as gynaecological cancers, has diagnosed these conditions and then referred the patient to the appropriate gynaecological cancer specialist. Associate Professor Kliman carried out his training at The Royal Women’s Hospital and in the United Kingdom and New York. He was the head of a number of units at The Royal Women’s Hospital and was a consultant and head of unit at The Royal Women’s Hospital for over 20 years.
Appointments can be made by phoning (03) 9419 2372 or by emailing info@drlenkliman.com.au or visiting the website.
Preparing For Your Gynaecological Visit
If you phone or email to make an appointment to see Associate Professor Len Kliman, one of our staff will take all your necessary details. She may ask you the reason for your visit as we often provide questionnaires to help us make a diagnosis. This information will be asked by one of our trained nursing staff. If you are already on treatment such as creams and lotions, it is best not to use them the night before your appointment. If besides your referral from your general practitioner you have any other results such as blood results, results of swabs or radiological results such as a previous pelvic ultrasound, it is wise to bring these along with you. You will be treated with respect and dignity. If any procedure is required such as looking at the vulval skin with a microscope, there will always be a nurse present in the rooms. Associate Professor Kliman always leaves the room when you undress and you will be given an appropriate gown and covered with a blanket during your examination. Both Associate Professor Kliman and our staff go out of their way to make sure that you feel comfortable and not stressed during your appointment.